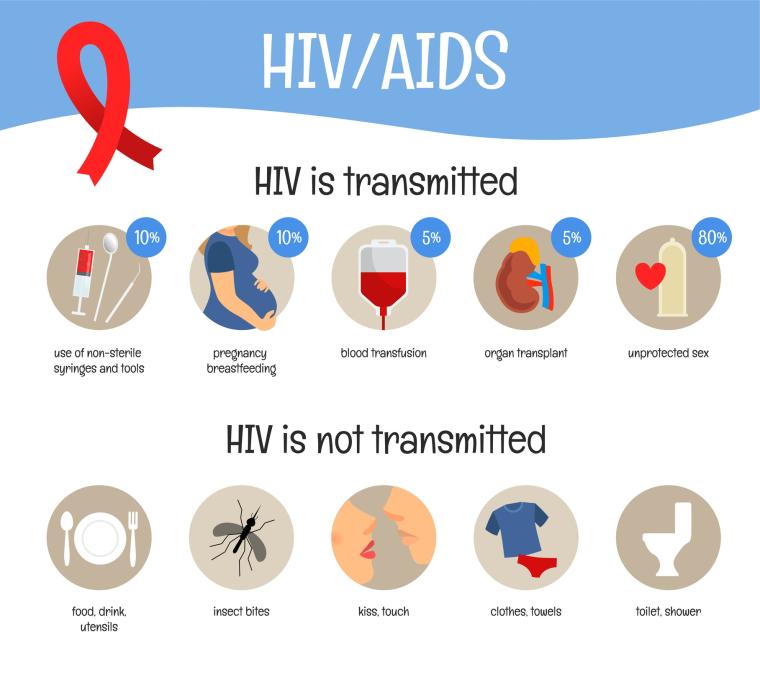
About HIV/AIDS
Preventing the spread of HIV/AIDS requires a collaborative effort between partners at the national, state, and local levels. CDC offers many resources for partners to use in their education and prevention efforts. Explore the options below to learn more about the basics of HIV and AIDS.